Understanding Bilateral Oophorectomy and Salpingectomy
Bilateral oophorectomy and salpingectomy are two surgical procedures that play a crucial role in women's reproductive health. These surgeries can be life-changing, and they are often recommended for various medical conditions. This article delves into what these procedures entail, their indications, recovery processes, and the implications for future health and wellness.
What is Bilateral Oophorectomy?
A bilateral oophorectomy refers to the surgical removal of both ovaries. This procedure is typically performed by a qualified obstetrician/gynecologist (OB/GYN) and can be indicated for a variety of reasons, including:
- Ovarian Cancer: One of the most significant reasons for a bilateral oophorectomy is the presence of ovarian cancer. Removing the ovaries can reduce the risk of cancer spread.
- Endometriosis: This painful condition occurs when tissue similar to the lining inside the uterus grows outside it. A bilateral oophorectomy may be recommended if other treatments have failed.
- Genetic Predisposition: Women with a family history of ovarian or breast cancer may choose to have this procedure to reduce their risk significantly.
- Severe Pelvic Pain: In cases where pain is unmanageable and linked to ovarian dysfunction, removal of the ovaries may be considered.
What is Salpingectomy?
A salpingectomy involves the removal of one or both fallopian tubes. This procedure can be performed laparoscopically, offering benefits such as reduced recovery time and minimal scarring. Reasons for a salpingectomy include:
- Ectopic Pregnancy: This occurs when a fertilized egg implants outside the uterus, typically in a fallopian tube. Emergency removal may be necessary to prevent complications.
- Tubal Cancer: The presence of cancerous cells in the fallopian tubes may necessitate a salpingectomy.
- Sterilization: Women may opt for a salpingectomy as a permanent method of contraception.
- Prevention of Cancer: Emerging studies suggest that removing the fallopian tubes can reduce the risk of certain types of cancers.
The Importance of These Procedures
Both bilateral oophorectomy and salpingectomy are significant for women’s health, not only for treating medical conditions but also for preventive measures against cancer.
Research has shown that women who undergo a salpingectomy before undergoing in vitro fertilization (IVF) may lower their risk of developing ovarian cancer in the future. The connection between the fallopian tubes and the development of ovarian cancer is an area of extensive study, and many health professionals are advocating for awareness regarding these procedures as preventive strategies.
Procedure Overview
Understanding what to expect from these surgeries can alleviate anxiety and prepare patients for the experience. Here’s a detailed breakdown:
Preparing for Surgery
Prior to surgery, patients will undergo comprehensive assessments, including:
- Medical History Review: It’s essential for the physician to know any underlying health conditions or medications.
- Imaging Tests: Ultrasounds or CT scans may be conducted to visualize the reproductive organs.
- Discussion of Risks: Patients should be informed about the risks and benefits of the surgery.
The Surgical Procedure
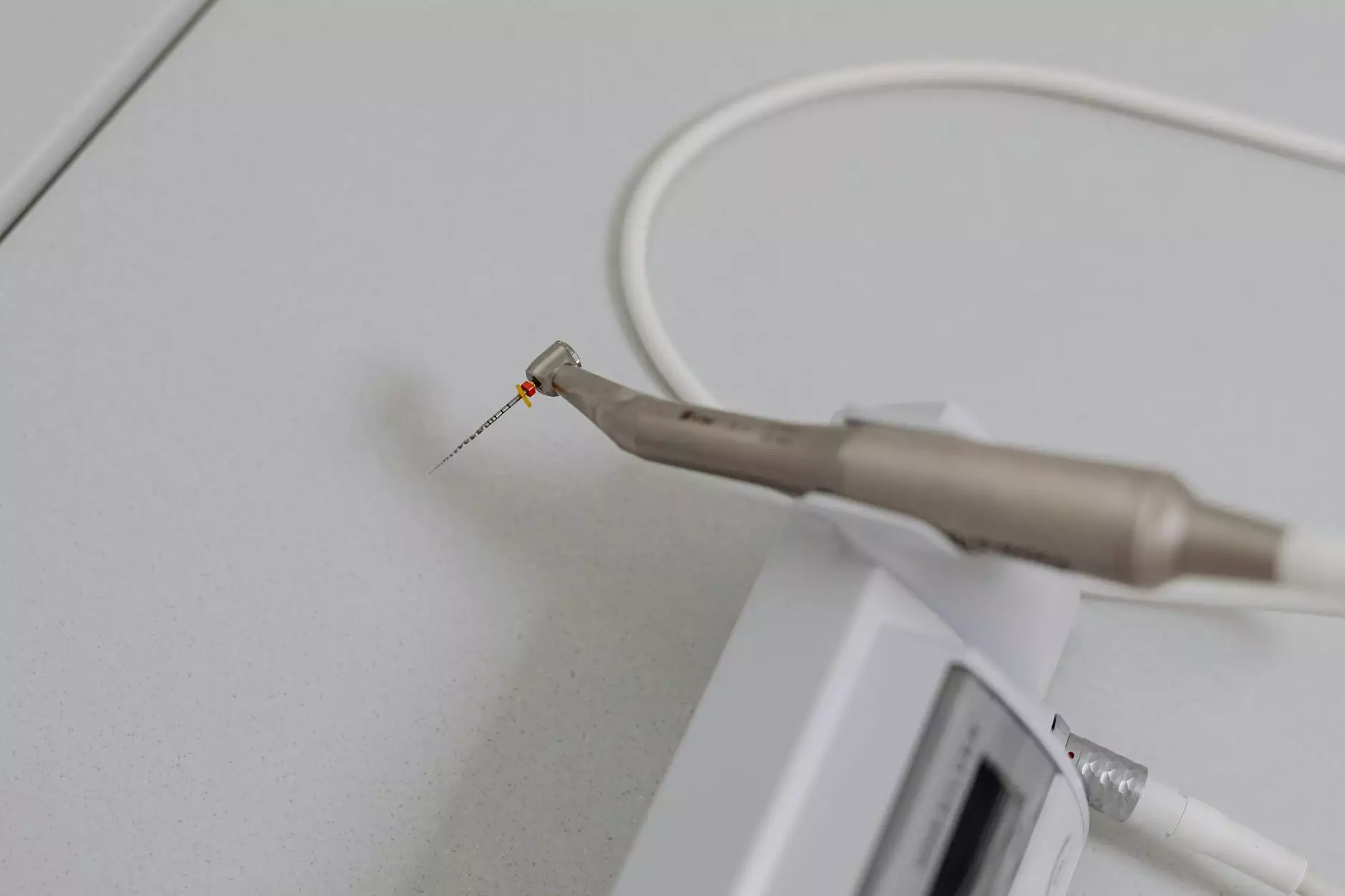
Both procedures are commonly performed under general anesthesia and can be done via laparoscopic or open surgical methods. Here are the steps generally involved:
- Anesthesia: The patient is given anesthesia to ensure comfort during the procedure.
- Incision: For laparoscopic procedures, several small incisions are made in the abdomen. For open surgery, a larger incision may be required.
- Removal: The surgeon carefully removes the ovaries or fallopian tubes as indicated.
- Closure: The incisions are then closed using sutures or staples, and a bandage is applied.
Recovery Process
The recovery time can vary based on the surgical method used but generally includes:
- Hospital Stay: Most patients will stay in the hospital for a day or two post-surgery.
- Rest and Care: Adequate rest and limiting physical activity are essential for recovery.
- Follow-Up Appointments: Regular check-ups with the healthcare provider will be necessary to monitor recovery.
Potential Risks and Complications
Like any surgical procedure, bilateral oophorectomy and salpingectomy come with potential risks, including:
- Infection: Increased risk of infection at the incision sites.
- Blood Clots: Postoperative blood clots can occur, especially in immobilized patients.
- Anesthesia Risks: Adverse reactions related to anesthesia can occur, although these are rare.
- Hormonal Changes: Women undergoing bilateral oophorectomy may experience sudden menopause.
Long-Term Health Implications
Following these surgeries, women may need to consider:
- Hormone Replacement Therapy (HRT): For those who have had a bilateral oophorectomy, HRT might be recommended to manage menopausal symptoms.
- Regular Health Check-Ups: Continuous monitoring of overall health is essential, as hormonal changes can lead to other health issues.
- Emotional Support: It's crucial for women to seek emotional and psychological support post-surgery as they navigate these significant lifestyle changes.
Conclusion
In summary, the procedures of bilateral oophorectomy and salpingectomy are vital surgical options for many women facing health issues related to their reproductive system. Understanding these procedures helps empower women to make informed decisions about their health.
If you or someone you know is considering these surgeries, consult with a qualified healthcare provider to discuss the best options tailored to individual health needs. At drseckin.com, we prioritize patient education and provide expert care tailored to women's unique health requirements.
bilateral oophorectomy salpingectomy








