Understanding Varicose Vein Removal: A Comprehensive Guide

Varicose veins are a common condition affecting millions of people around the world. These swollen, twisted veins often appear on the legs and can be both a cosmetic concern and a source of discomfort. Understanding varicose vein removal is crucial for those seeking relief from this condition. This article will delve into what varicose veins are, their causes, the available removal treatments, recovery processes, and preventive measures. Let's navigate through the world of vascular health together.
What Are Varicose Veins?
Varicose veins are veins that have become enlarged and twisted. They often exhibit a dark purple or blue hue and can be easily seen through the skin. These veins develop when the valves inside the veins weaken, causing blood to pool rather than circulate effectively. This results in increased pressure within the veins, leading to their enlarged appearance. Common symptoms include:
- Pain or aching in the legs, especially after standing for long periods.
- Swelling in the legs and ankles.
- Itching or irritation of the skin surrounding the affected veins.
- Skin discoloration or changes in the texture of the skin around the ankles.
Causes of Varicose Veins
Several factors contribute to the development of varicose veins:
- Genetics: A family history of varicose veins greatly increases your risk.
- Age: As we age, our veins can lose elasticity, making them more prone to varicosity.
- Gender: Women are more likely than men to develop varicose veins due to hormonal changes, especially during pregnancy.
- Obesity: Excess weight puts added pressure on veins in the legs.
- Prolonged standing or sitting: Occupations that require long periods of standing or sitting can impair circulation.
Diagnosis of Varicose Veins
Diagnosing varicose veins is usually straightforward. A healthcare provider, often a vascular specialist, will conduct a physical examination and may also use ultrasound imaging to assess the blood flow in the veins. This assessment helps determine the severity of the condition and guides appropriate treatment options.
Exploring Treatment Options for Varicose Vein Removal
Numerous treatments are available for varicose vein removal, ranging from lifestyle changes to medical procedures. Understanding these options is essential for making an informed decision about your health:
1. Lifestyle Changes
For mild cases, lifestyle modifications can significantly improve symptoms:
- Weight Management: Losing weight can reduce pressure on the veins.
- Regular Exercise: Engaging in activities like walking or swimming promotes better circulation.
- Compression Stockings: These supportive garments help reduce swelling and discomfort.
2. Minimally Invasive Procedures
For more pronounced varicose veins, minimally invasive procedures offer effective solutions:
- Endovenous Laser Treatment (EVLT): A laser is used to seal off the affected veins, redirecting blood flow to healthier veins.
- Radiofrequency Ablation: Similar to EVLT, this method uses radiofrequency energy to close varicose veins.
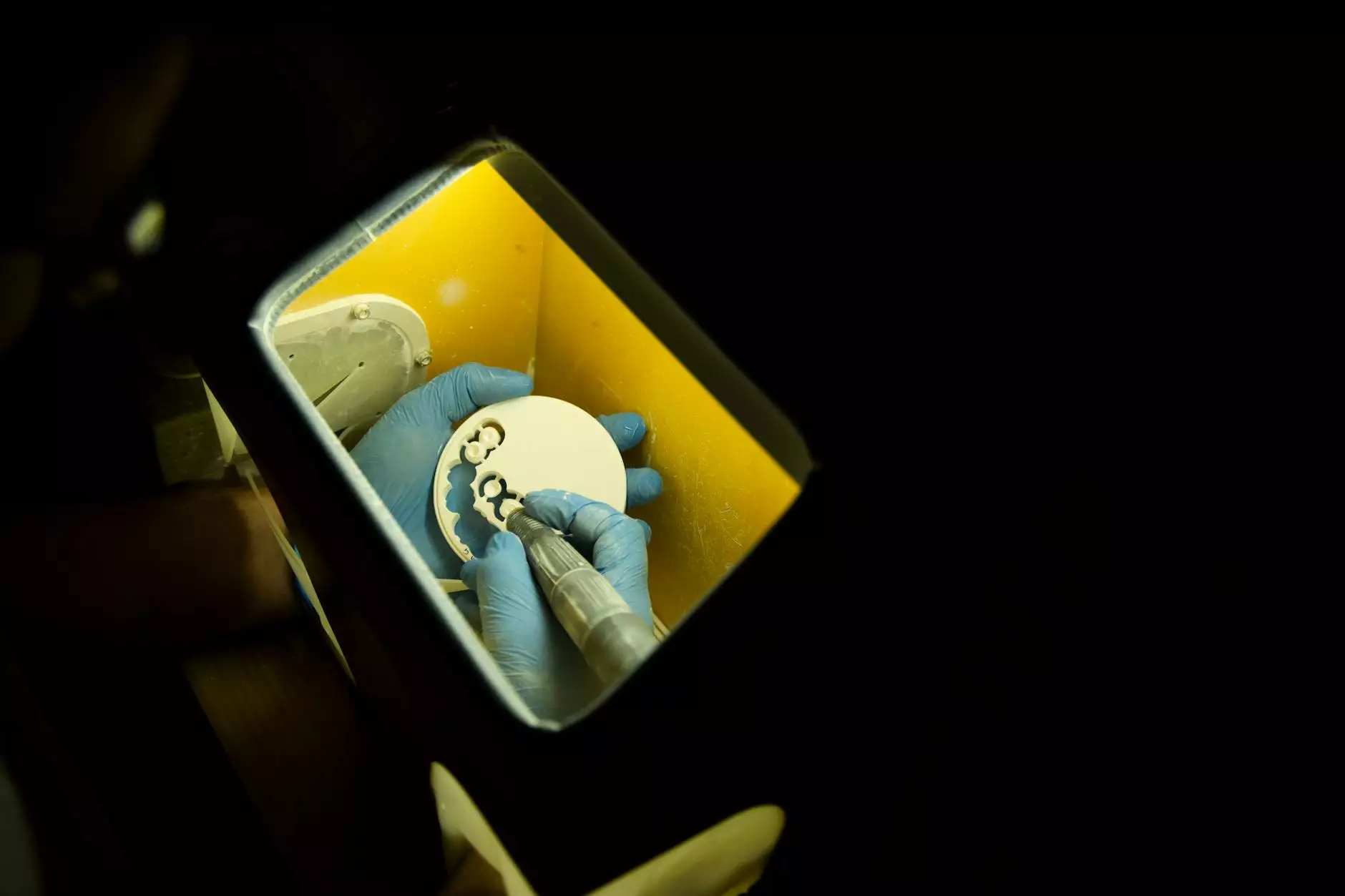
- Sclerotherapy: A solution is injected into the vein, causing it to scar and close.
3. Surgical Options
In more severe cases, surgical interventions may be necessary:
- Vein Stripping: A traditional surgery where the problematic vein is removed from the leg.
- Ambulatory Phlebectomy: Small incisions are made to remove varicose veins, typically used for surface veins.
Recovery and Aftercare
The recovery time after varicose vein removal procedures varies depending on the method used:
- Minimally Invasive Procedures: Patients often resume normal activities within a few days but should avoid heavy lifting and strenuous exercise for at least a week.
- Surgical Procedures: Recovery might take longer, usually a couple of weeks, with follow-up appointments to monitor healing.
Regardless of the method, following your physician’s aftercare instructions is vital for optimal recovery and minimizing complications.
Potential Risks and Complications
Like any medical procedure, varicose vein removal comes with potential risks. These may include:
- Infection: There is a risk of infection at the incision sites.
- Blood Clots: Although rare, blood clots can form in the treated veins.
- Changes in Skin Color: Some patients may experience discoloration in the treatment area.
Discussing these risks with your healthcare provider can help you weigh the benefits against potential downsides.
Preventing Varicose Veins
While not all varicose veins can be prevented, certain measures can reduce your risk:
- Maintain a Healthy Weight: Keeping your body weight in check can lessen the burden on your vascular system.
- Stay Active: Regular physical activity helps with circulation and vein health.
- Avoid Long Periods of Inactivity: If your job requires extended sitting or standing, take breaks to move and stretch.
- Elevate Your Legs: When resting, elevate your legs to improve circulation.
Conclusion
Understanding varicose veins and the options available for varicose vein removal is an empowering step towards better vascular health. Whether through lifestyle changes, minimally invasive treatments, or surgical procedures, there is a viable path to relief. Always consult with a qualified vascular specialist, like those at Truffles Vein Specialists, to discuss your symptoms, potential treatments, and recovery processes. Embrace the journey to healthier veins and a more comfortable lifestyle.